Opioid Withdrawal: How Long Does It Last?
Opioid withdrawal is the process that the body undergoes when someone dependent on opioids, such as prescription painkillers or heroin, stops or reduces their usage. It occurs as the body adjusts to the absence of these substances, leading to various physical and psychological symptoms.
The duration of opioid withdrawal can vary from one person to another, depending on different factors. Generally, withdrawal unfolds in three distinct stages: early, peak, and late. Continue reading as we explore these stages in detail and effective ways to deal with associated distressing symptoms.
Key Takeaways
Opioid withdrawal occurs when someone dependent on opioids stops or reduces their usage. Here is what you need to know:
- Opioid withdrawal unfolds in three stages, each marked by unique challenges.
- The duration of opioid withdrawal can vary from one person to another, depending on various factors.
- Effective opioid withdrawal management strategies are available, including an opioid detox program.
For those struggling with substance use disorder (SUD), seek professional help at The Haven Detox-New Jersey—call (856) 565-3102 for more information.
Understanding Opioid Withdrawal
Opioids are a class of drugs that include both prescription drugs, such as oxycodone, hydrocodone, and morphine, as well as illicit drugs like heroin. These drugs are commonly prescribed for pain management due to their powerful analgesic effects.
However, misuse or prolonged use of opioids can lead to the onset of tolerance, dependence, and addiction. When someone with opioid dependence abruptly reduces or ceases their opioid use, they may experience a set of symptoms collectively known as opioid withdrawal.
Opioid withdrawal is a challenging and uncomfortable process that reflects the body’s attempt to readjust to the absence of opioids. The severity and duration of opioid withdrawal can vary depending on various factors. Medical detoxification and supportive care are often recommended to manage opioid withdrawal safely and effectively.
Opioid Withdrawal Timeline: Exploring the Stages
Opioid withdrawal is a challenging journey, marked by distinct stages that individuals may encounter. Knowing what to expect can empower both those experiencing withdrawal and their support networks.
Let’s break down the stages of opioid withdrawal into three phases:
Early Withdrawal Symptoms
Typically, withdrawal begins within the first 6-12 hours after the last opioid use. Early withdrawal symptoms are often mild initially but can escalate quickly. The initial withdrawal symptoms may include:
- Anxiety and restlessness
- Insomnia
- Sweating
- Yawning
- Runny nose and teary eyes
- Muscle aches and pains
- Increased heart rate
- Dilated pupils
- Gastrointestinal symptoms (such as nausea, vomiting, diarrhea)
Peak Withdrawal Symptoms
Generally, peak withdrawal symptoms occur within 1-3 days after the last opioid use. This is the most intense phase. Individuals may experience:
- Severe cravings for opioids
- Intense anxiety and agitation
- Goosebumps
- Sweating and chills
- Muscle spasms and abdominal cramps
- Nausea, vomiting, and diarrhea
- Insomnia
- Increased blood pressure and heart rate
Late Withdrawal Symptoms
Typically, late withdrawal symptoms persist for several days to weeks, gradually improving over time. The common withdrawal symptoms in this stage may include:
- Lingering anxiety and depression
- Fatigue and low energy
- Difficulty concentrating
- Irritability
- Insomnia or disrupted sleep patterns
- Continued cravings for opioids
- Gastrointestinal issues
Each phase comes with its unique set of struggles, but with the right support and mindset, recovery is achievable. Remember, seeking professional help and leaning on a supportive community are vital components of the journey toward a drug-free life.
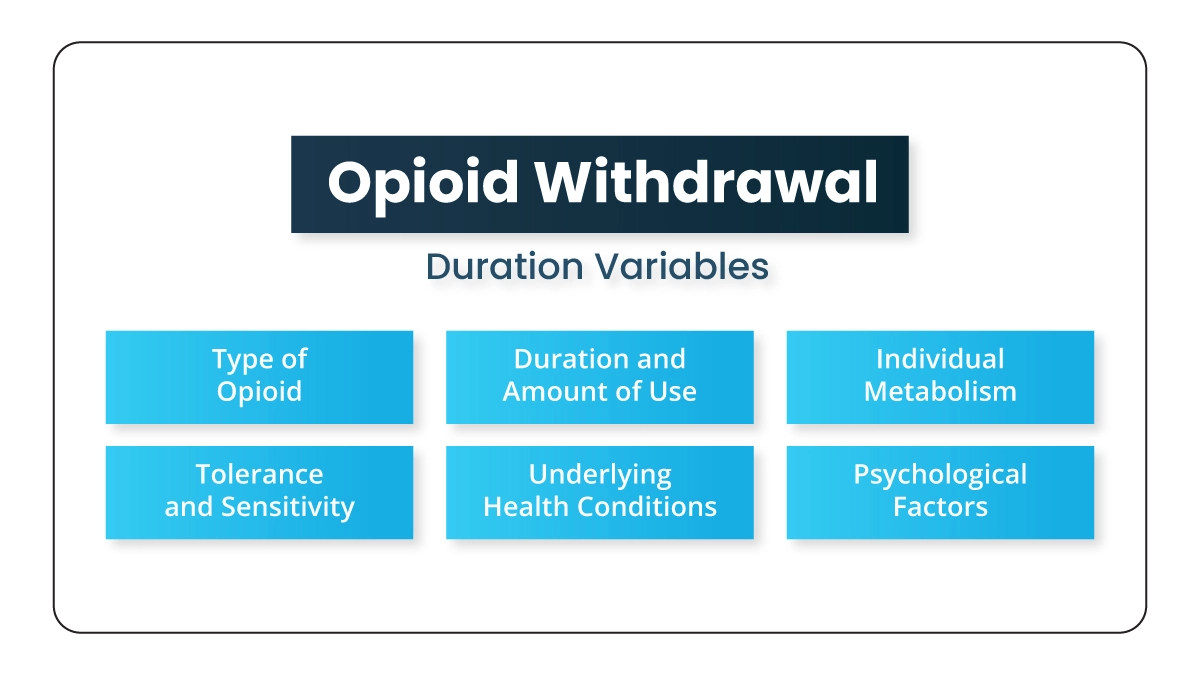
Opioid Withdrawal Duration Variables
The duration and severity of opioid withdrawal can vary among individuals due to a combination of factors. Here’s a breakdown of some key factors that influence the duration of opioid withdrawal:
Type of Opioid
The specific opioid at the center of the withdrawal process plays an important role in determining its duration. Different opioids have varying half-lives and potencies, leading to differences in withdrawal duration. Short-acting opioids may prompt a more rapid onset of withdrawal symptoms compared to long-acting opioids.
Duration and Amount of Use
The duration and quantity of opioid use are pivotal factors in withdrawal duration. Prolonged and high-dose usage often results in more intense withdrawal symptoms that may persist for an extended period. Abrupt cessation after prolonged use can trigger a more protracted withdrawal timeline.
Individual Metabolism
Individual metabolic rates play a vital role in drug processing and elimination from the body. Variations in metabolism contribute to differences in how quickly opioids are cleared, influencing the onset and duration of withdrawal symptoms.
Tolerance and Sensitivity
The development of tolerance, wherein the body adapts to the presence of opioids, and individual sensitivity to symptoms of withdrawal can impact the overall withdrawal experience. Higher tolerance levels may extend the withdrawal phase.
Method of Administration
The method of administration affects the speed at which opioids enter the bloodstream. Intravenous or smoked administration may result in a quicker onset of withdrawal symptoms compared to orally administered opioids.
Individual Differences
Genetic factors, age, and overall health contribute to individual variations in opioid withdrawal. Genetic predispositions may influence how the body responds to opioids, impacting the duration and intensity of withdrawal symptoms.
Underlying Health Conditions
Pre-existing health conditions can exacerbate withdrawal symptoms. Individuals with compromised health may experience prolonged or intensified withdrawal due to the interplay of opioid effects with their underlying health issues.
Psychological Factors
Psychological aspects, including the individual’s mental state, motivation, and coping mechanisms, can influence the perception and endurance of withdrawal symptoms. Mental health plays an essential role in navigating the challenges of withdrawal.
Remember, opioid withdrawal experiences are highly individual, and the interplay of these factors can result in a wide range of responses.
Withdrawal Complications
Opioid withdrawal symptoms can be challenging but are generally not life-threatening. However, complications may arise, especially if withdrawal is severe or if the individual has underlying health issues. Complications may include:
Dehydration
Diarrhea, vomiting, and excessive sweating are common symptoms of opioid withdrawal. These can lead to dehydration, which may require medical attention to restore fluid balance.
Electrolyte Imbalance
Loss of fluids through vomiting and diarrhea can result in electrolyte imbalances, such as low potassium, sodium, and magnesium levels. Severe imbalances can affect the heart and other vital organs.
Cardiovascular Complications
Opioid withdrawal can result in cardiovascular issues, including an increased heart rate and high blood pressure. In some cases, especially if there are pre-existing heart conditions, these changes can pose risks.
Gastrointestinal Issues
Nausea, vomiting, and diarrhea are common during opioid withdrawal and can lead to nutritional deficiencies. Prolonged vomiting and diarrhea may require medical intervention to prevent complications.
Mental Health Effects
Opioid withdrawal can have a significant impact on mental health, leading to symptoms such as anxiety, depression, irritability, and difficulty concentrating. In some cases, severe emotional distress may require emotional support.
Severe Withdrawal Symptoms
In some instances, individuals may experience severe withdrawal symptoms, such as seizures or hallucinations. These can be dangerous and require immediate medical attention.
Relapse Risk
The discomfort of withdrawal may drive individuals to seek relief by returning to opioid use. This can lead to overdose, especially if the person underestimates the dosage needed to achieve the desired effect.
Medical Complications
People with pre-existing medical conditions, such as heart problems or respiratory issues, may experience worsened symptoms during withdrawal. Individuals with underlying health concerns must be closely monitored during the withdrawal process.
Suicidal Thoughts
Opioid withdrawal can contribute to mental health challenges, and in some cases, individuals may experience suicidal thoughts. Proper support, including mental health care, is crucial to address these concerns.
If you or someone you know is experiencing opioid and opiate withdrawal, seeking medical attention is crucial for a safer and more comfortable withdrawal process.
Dealing with Opioid Withdrawal: Effective Strategies
Opioid withdrawal can be a challenging and daunting experience, but there are various effective strategies to manage and overcome these symptoms. The most common ones include:
Medically Supervised Detoxification
The important first step in overcoming opioid withdrawal is often medically supervised detoxification. This process involves the removal of opioids and opiates from the body in a controlled environment. Medical professionals administer medications to ease withdrawal symptoms and ensure the safety of the individual during this critical phase.
Rehabilitation Programs
Rehab programs provide structured environments for individuals recovering from opioid addiction. Inpatient programs offer immersive, 24/7 care in a medical treatment facility, while outpatient programs allow individuals to receive treatment while maintaining their daily responsibilities. Both options include a combination of medical support, therapy, and counseling.
Medication-Assisted Treatment (MAT)
Medication-assisted treatment (MAT) involves the use of medications approved by the United States Food and Drug Administration (FDA), such as methadone, buprenorphine, or naltrexone, to help manage opioid withdrawal symptoms and cravings. This approach, when combined with counseling and therapy, has shown effectiveness in supporting long-term recovery.
Therapy and Counseling
Therapy and counseling play a crucial role in addressing the psychological aspects of addiction. Individual and group therapy sessions help individuals explore the root causes of their substance abuse, develop coping skills, and build a support network. Cognitive behavioral therapy (CBT) is particularly effective in changing negative thought patterns and behaviors associated with opioid use disorder (OUD).
Support Groups
Peer support is invaluable during recovery. Support groups, like Narcotics Anonymous (NA) and SMART Recovery, offer a sense of community and understanding. Sharing experiences and receiving encouragement from others who have walked a similar path can be a powerful motivator.
Healthy Lifestyle Changes
Adopting a healthy lifestyle is integral to the recovery process. This includes regular exercise, proper nutrition, and adequate sleep. These lifestyle changes promote physical well-being and contribute to improved mental health and resilience during the recovery journey.
Holistic Approaches
Holistic approaches encompass alternative therapies such as yoga, meditation, acupuncture, and mindfulness. These practices address the mind-body connection, promoting overall well-being and aiding in the management of stress, anxiety, and other factors that may contribute to drug use disorder.
Remember, there is no one-size-fits-all solution; a combination of these strategies tailored to individual needs forms a robust foundation for successful opioid withdrawal and long-term recovery.

 (856) 565-3102
(856) 565-3102
